Description
A hand fracture is a break in one of the bones in the hand. This includes the small bones of the fingers (phalanges) and the long bones within the palm (metacarpals). A broken hand can be caused by a fall, crush injury, twisting injury, or through direct contact in sports.
In most cases, a hand fracture will heal well with nonsurgical treatment. Depending on the type and location of the fracture, this may include wearing a cast, splint or buddy straps for a period of time. For more serious fractures or for fractures that do not line up properly, however, surgery may be required to realign the broken pieces of bone.


AnatomyHello
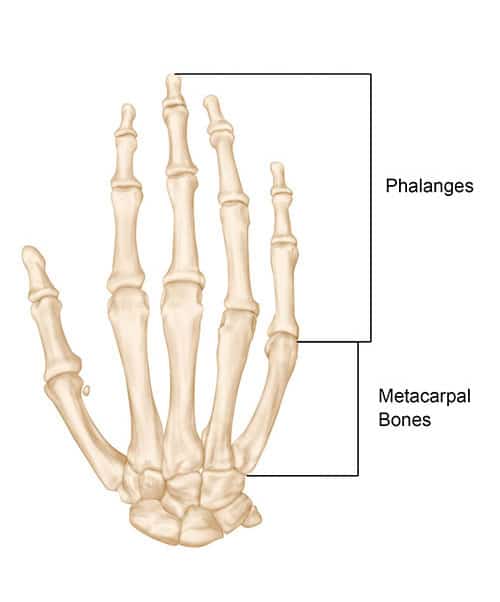
The bones in your hand include:
- Phalanges. These are the small bones that form the thumb and fingers. There are two phalanges in the thumb and three in each of the fingers.
- Metacarpals. These are the five bones that are located in the palm of the hand.
The most common hand fracture is a fracture of the fifth metacarpal—the bone in the hand that supports the little finger. This is commonly called a “boxer’s fracture” and involves the “neck” of the bone, next to the knuckle joint. A boxer’s fracture is caused most often by punching or striking a hard object when your hand is closed in a fist.
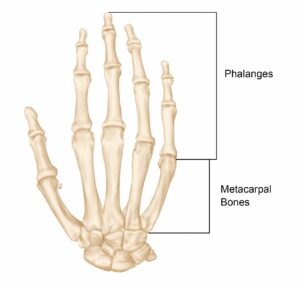
Figure: The bones of the hand. A fracture can occur in the middle of a bone or at the end, near the joint.
Reproduced from JF Sarwark, ed: Essentials of Musculoskeletal Care, ed 4. Rosemont, IL, American Academy of Orthopaedic Surgeons, 201
Signs and symptoms
Signs and symptoms of a hand fracture may include:
- Swelling
- Bruising
- Tenderness or pain
- Deformity
- Inability to move the finger
- Shortened finger
- The injured finger crosses or “scissors” over its neighbor when making a partial fist
In the case of a boxer’s fracture, the patient’s knuckle may look sunken in or depressed. This is caused by the displacement or angulation of the end or “head” of the metacarpal bone.

Figure: X-ray of a “boxer’s fracture” in the fifth metacarpal. This common hand fracture can cause the knuckle on the affected finger to appear sunken in or angulated.
Reproduced from Johnson TR, Steinbach LS (eds): Essentials of Musculoskeletal Imaging. Rosemont, IL American Academy of Orthopaedic Surgeons, 2004, p. 347.
Doctor Examination
Because a boutonnière deformity is only one of several injuries that result from a “jammed finger,” you should consult a doctor for an appropriate diagnosis and treatment. Your doctor will examine the fingers and hand. He or she will ask you to straighten the affected finger and bend the fingertip. X-rays may be recommended to detect any broken bones attached to the central slip of tendon.
Physical Examination
Your doctor will ask about your symptoms and perform a careful examination of your fingers and hand. During the exam, he or she will look for:
- Swelling or bruising
- Deformity
- Overlapping of your fingers
- Cuts or lacerations to the skin around the injury
- Limited range of motion
- Joint stability
- Numbness in your fingers, a sign of possible nerve damage
Typically, your doctor will evaluate the tendons in your hand to ensure they are functioning properly and will check for instability in the joint(s) near the fracture.
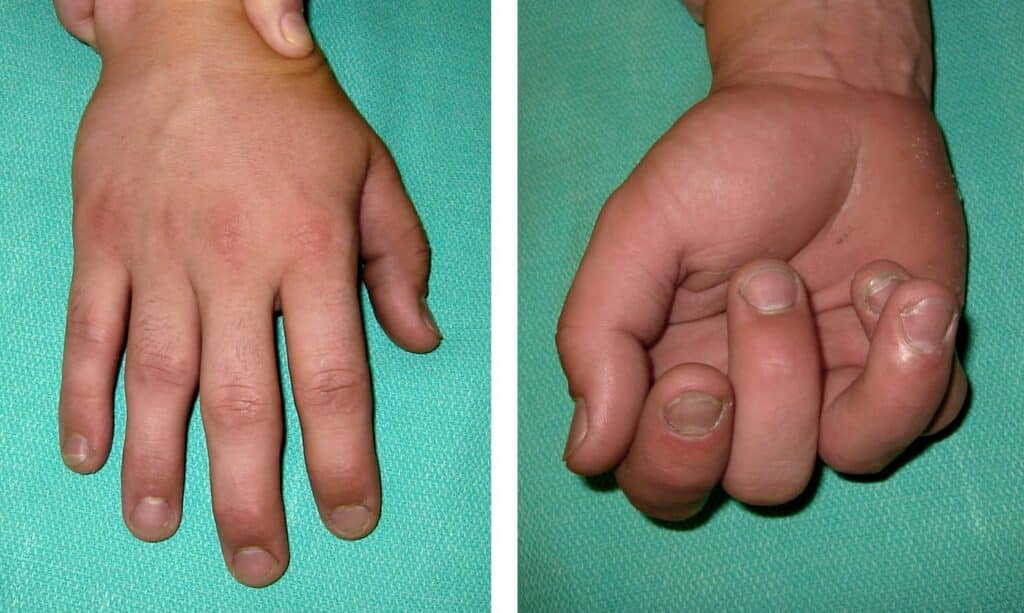
Figure: (Left) This patient’s fractured ring finger cannot be easily detected when his hand is fully extended. (Right) When he makes a partial fist, however, the fracture is more obvious. The fractured ring finger overlaps the adjacent little finger.
Reproduced and adapted from Lehman TP: Hand fractures: current concepts. Orthopaedic Knowledge Online Journal 2012; 10(3). Accessed June 2017.
X-rays
X-rays provide images of dense structures, such as bone. Your doctor may order one or more x-rays to help identify the location and extent of the fracture.

Figure: X-rays show a phalanx fracture (left) and a metacarpal fracture (right).
(Left) Reproduced from Kozin SH, Thoder JJ, Lieberman G: Operative Treatment of Metacarpal and Phalangeal Shaft Fractures. J Am Acad Orthop Surg 2000;8:111-121. (Right) Reproduced from Johnson TR, Steinbach LS (eds): Essentials of Musculoskeletal Imaging. Rosemont, IL American Academy of Orthopaedic Surgeons, 2004, p. 347.
Treatment
Nonsurgical Options
If a fracture does not line up in an acceptable position, often, your doctor can realign the bone fragments by gently manipulating them back into position without making an incision. This procedure is called a closed reduction. A cast, splint or brace may be applied to keep the bones in acceptable alignment while they heal. The cast may extend from your fingertips almost to your elbow to support the bones properly.
Your doctor will probably order a second set of x-rays about 1 to 2 weeks later. This is done to ensure that the bones are healing in the proper position.
Depending on the location and stability of the fracture, you may have to wear the cast for 3 to 6 weeks. Some types of fractures can be protected by wearing a removable splint or by being “buddy strapped” to an adjacent non-injured finger. The non-injured finger acts as a “moving splint” to support the injured finger.
Gentle hand exercises can usually begin after 3 weeks.
Surgical Options
Some hand fractures require surgery to realign and stabilize the fracture fragments. This includes open fractures in which pieces of bone have broken through the skin.
Your doctor will make an incision to help reposition the bone fragments into their normal alignment. Small metal devices—such as wires, screws, pins, staples, and plates—may be used to hold the pieces of fractured bone in place.

Figure: (Left) X-ray shows a metacarpal fracture of the ring finger. (Right) Here, the fracture has been repaired with a plate and screws.
Reproduced from Kozin SH, Thoder JJ, Lieberman G: Operative Treatment of Metacarpal and Phalangeal Shaft Fractures. J Am Acad Orthop Surg 2000;8:111-121.
After surgery, you may have to wear a splint or cast for a period of time in order to protect the fracture. If the bone changes position during healing, your finger may lose some function. Your doctor will talk with you about when it is safe to begin range-of-motion exercises and to resume your activities after surgery.

Figure: (Left) X-ray shows fractures in the phalanges of two fingers. (Right) In this x-ray, the fractures have been repaired with screws.
Reproduced from Kozin SH, Thoder JJ, Lieberman G: Operative Treatment of Metacarpal and Phalangeal Shaft Fractures. J Am Acad Orthop Surg 2000; 8:111-121.
Complications of Hand Fractures
Because some fractures require prolonged immobilization in a cast or splint, your hand and fingers may become stiff. Your doctor or, in some cases, an occupational therapist, physical therapist or hand therapist, will provide specific exercises to help decrease stiffness and improve function.
Even after carefully following therapy instructions after fracture treatment, some patients may continue to have difficulty with stiffness or a contracture (loss of motion) in the hand. If this occurs, your doctor may recommend a surgical procedure to help restore motion and/or function to your finger. Commonly used procedures include:
- Surgical removal of the retained hardware (such as pins, screws, or plate and screws)
- Tenolysis—freeing up a tendon from scar tissue
- Contracture release—releasing the tight or restrictive supporting structures around the involved joint, including the ligaments and/or joint capsule
Generally, these procedures are used once a fracture has healed and there is no evidence of progress or improvement in the return of function to the injured finger. Your doctor will talk with you about whether an additional procedure is needed in your situation and how it may affect your recovery.
