Description
A “jersey finger” refers to a rupture of the flexor tendon, which is the tendon that bends the fingertip down. Its name comes from football athletes who have gripped the jersey of an opposing player who is trying to get away. As the player tries to free themselves, the finger gets unexpectedly straightened as it is still trying to flex and grip.
This creates a tug of war, where the tendon is being pulled in two directions. This can result in the tendon separating from its bone insertion at the tip of the finger.
Sometimes, a piece of the bone is torn away as well. While this example is classic, other sports and activities (e.g. rock climbing) can lead to a jersey finger.
Most of the tendons that move your fingers originate in the forearm. The flexor digitorum profundus (FDP) muscle (Figure 1), is responsible for bending the fingertip down. Therefore, the medical term for a “jersey finger” is FDP avulsion. There are three types: type I, II or III. Type I is the most severe (total retraction of tendon into the palm).
Type III is the most favorable. This has little to no retraction of tendon. There is a blood supply to the flexor tendon at each joint.
Thus, when the tendon is retracted further away from the tip toward the base of the finger, more of the blood supply is disrupted. Loss of blood supply can affect how fast you heal and how successful your treatment may be.
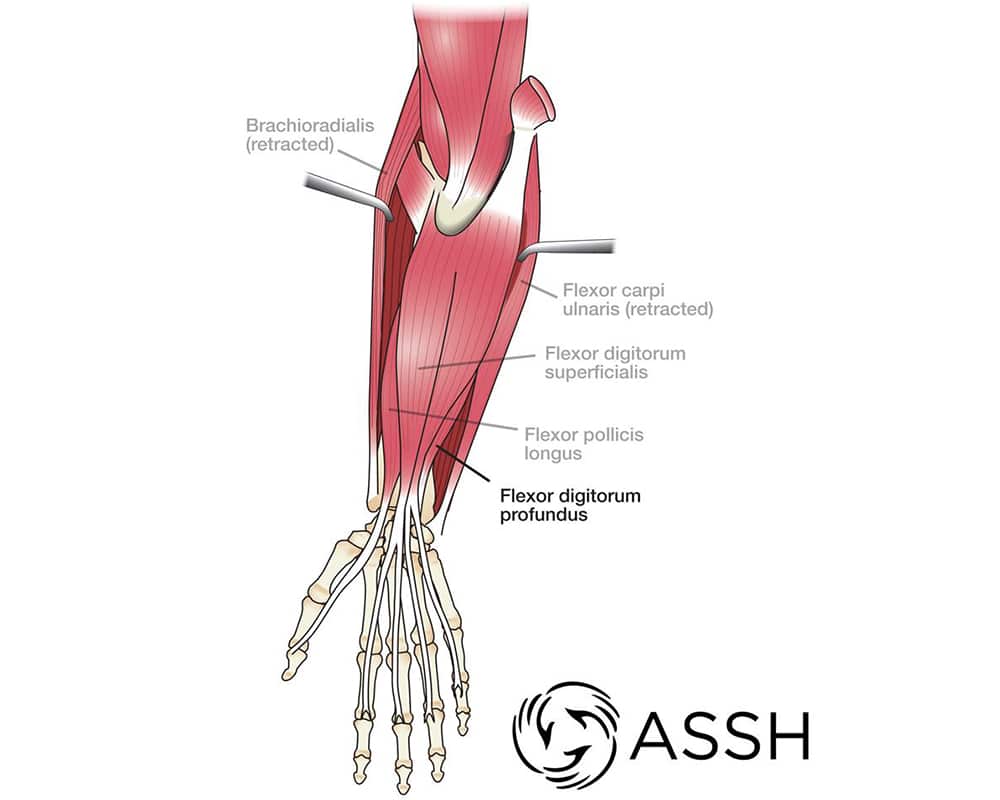
Figure 1 : The flexor digitorum profundus (FDP) muscle
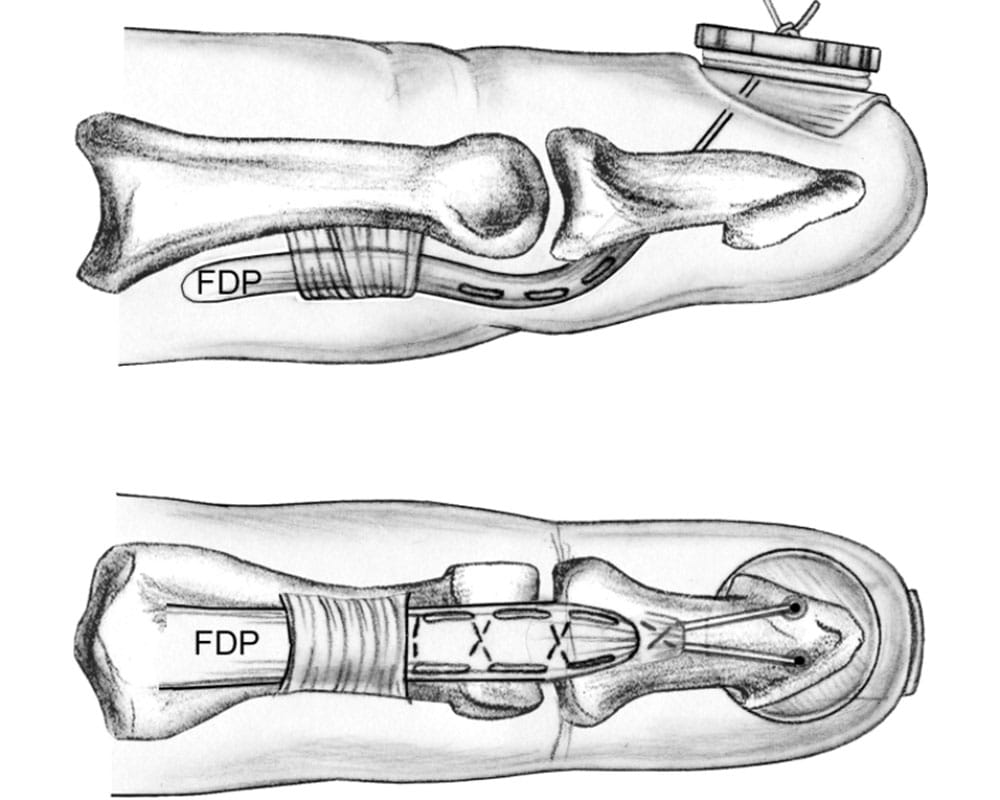
Figure 3 : Suture-button surgical method

Figure 2 : A ring finger unable to bend due to jersey finger
Figure 4 : A splint to be worn after surgery
Signs and SymptomsHe
With a jersey finger, the injured finger is unable to bend at the fingertip, even though the finger may be able to bend at the other joints (Figure 2). The fingertip may be swollen and painful, depending on how the injury occurred and how much time has passed since the injury.
People often report hearing or feeling a “popping” sensation at the time of injury. The ring finger is most often involved, but any finger can be affected. If there is a lot of pain in the palm just before the base of the finger, it may be a sign of a Type 1 rupture.
Doctor Examination
The diagnosisis often made based on history and physical examination alone. Many times, patients and other physicians that don’t specialize in hand surgery may miss a jersey finger. They will see that the first two finger joints are bending and not recognize that the finger tip is not moving. Other times it may be noticed the fingertip is not moving, but people think the motion loss is due to pain or swelling.
During the diagnosis, your hand surgeon may try to isolate your movement by holding your knuckle joint straight to prevent it from bending and seeing if you can move the fingertip. If it does not move, you likely ruptured the tendon. Your doctor may order x-rays to see if a piece of bone has chipped off with the disrupted tendon.
Treatment
Boutonnière deformity must be treated early to help you retain the full range of motion in the finger.
Nonsurgical Options
The treatmentdepends on your injury. If there is a broken bone (fracture) along with the jersey finger, your treatment may be different. The majority of these injuries benefit from surgery to reattach the disrupted tendon, fix the bony fracture (if necessary), and restore the ability to bend the finger tip. This is particularly true in young, active patients and athletes.
Surgical Options
Some people may prefer to avoid surgery, either due to underlying medical conditions or an inability or unwillingness to comply with post-surgery requirements such as taking it easy and/or receiving hand therapy. However, the inability to bend the finger tip will likely be permanent without surgery. Talk to your hand surgeon about the best treatment for you. It can take several months for the tendon to gain enough strength to return to normal activities.
What to expect with surgery
The timing of surgery after your injury depends on whether there is an associated bony fracture and how far the disrupted tendon has retracted. It is important to consult a hand surgeon as soon as possible after your injury because delayed assessment and treatment can lead to a more difficult recovery.
There are various surgical methods to reconstruct the disrupted tendon. Your surgeon will likely choose from one of a few methods to make the repair; these options may include the suture-button method (depicted in Figure 3) or methods utilizing internal bone anchors. If there is an associated fracture, it may need to be repaired with pins or screws. Your surgeon will help guide you in choosing the appropriate method of reconstruction based on your individual injury pattern.
After surgery, you will likely be put in a splint for a period of time, possibly like the splint depicted in Figure 4. This will vary depending on the severity of injury, type of repair, and rehabilitation preferences of your surgeon. You will most likelybe required to do home exercises carefully chosen by your surgeon. Some patients may require therapy from a certified hand therapistto prevent stiffness and restore range of motion. These injuries, including the surgery and rehabilitation, are complex. Too much activity too soon may not lead to a good recovery. On the other hand, not enough motion soon enough could result in stiffness. Sometimes a secondary surgery is needed, called a tenolysis, if your motion is limited.
