- Hand Surgery Anesthesia
- Cortisone Shots
- Hand and Finger Exercises
- Hand / Occupational Therapy
- Heat and Cold Treatment
- Opioid Information
- Pain Management After Surgery
- Scar Treatment
- Splint and Cast Care
Hand Surgery Anesthesia
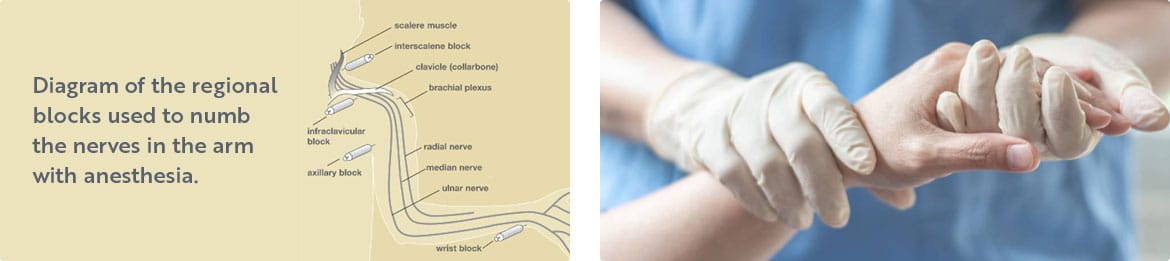
Anesthesia is a way to control pain during a surgery or procedure using medication. The types of medications used for this purpose are called anesthetics. Anesthesia can help control breathing, blood pressure, and heart rate.
There are several types of anesthesia for patients undergoing hand surgery. These include local, regional, or general anesthesia. The type used depends on several factors. Surgical factors, including the type and length of the surgery are assessed. The patient’s health and other medical conditions are also assessed. Also considered are the preferences of the patient, surgeon, and anesthesiologist. Together, the patient and the treatment team decide on a type of anesthesia.
General Anesthesia
With general anesthesia, the patient is unconscious and does not feel anything during the surgery. With this type of anesthesia, the patient requires airway and breathing support from a ventilator. This is due to the type of gas they are inhaling (or medication in their IV) that puts them to sleep.
Local Anesthesia
This typically means anesthetics for a small area. Numbing medicine is injected at the site of surgery. There are different types of local anesthetic medications that last for different amounts of time. Some may last for only 1 or 2 hours and others may last for 8 or more. When local anesthesia is used alone, the patient is wide-awake during the surgery. The patient can cooperate with instructions from the surgeon. Sometimes the surgeon may ask the patient to move the hand or fingers to see if a finger is still triggering or to check the tension on a tendon repair. Sometimes epinephrine may be mixed with the local anesthetic to limit excessive bleeding. This may make the skin look pale where the medication is injected.
Monitored Anesthesia Care (Sedation)
This type of anesthesia helps you relax by giving medication through an IV line. The medicines often make you lose your short-term memory. You often don’t remember being in surgery, even though you could be awake and talk at times during the surgery. With this type of anesthesia, you breathe on your own, so you don’t need a breathing tube. This helps reduce the risk of having a sore throat. This type of anesthesia is often given by the anesthesia team in combination with local anesthetics injected by the surgeon.
Regional Anesthesia
With regional anesthesia, parts of the body are put to sleep by injecting numbing medicine through a needle placed along the path of nerves. This may be around the collarbone or neck, under the arm, at the wrist, in the palm, or around the finger. It may also be through an IV in the arm. Regional anesthesia uses numbing medications that can provide between one and 24 hours of pain relief. As with local anesthesia, relaxing medication may be given through an IV line. Many times, ultrasound is used to visualize blood vessels, landmarks, and nerves. Other times a nerve stimulator is used to help place the medication close to the nerves. This causes the arm or hand muscles to twitch and move, which while not painful can feel strange. To limit pain during the injection of numbing medicine with a needle, IV medication may be given to help you relax and feel comfortable. Some benefits of this type of anesthesia include less need for pain medicine after surgery. It has also been linked to faster recovery and less nausea. For some surgeries, regional anesthesia is linked to less blood loss and lower risk of blood clots.
Will I be Awake During Surgery?
Some patients prefer to be awake during surgery. Others prefer to be asleep. During your surgery you can be awake or asleep, depending on what type of anesthesia you and the treatment team decide on. You will not be able to see the surgery itself because of the large sterile drape placed between you and the surgeon. This is to protect the “sterile field.” The “sterile field” is the important area of your surgery, kept clean and free from germs that can cause infection.
What Are the Risks?
Some risks associated with regional or local anesthesia include pain, soreness or bruising at the needle site. Sometimes a pupil changes size, muscles that move the diaphragm may get numbed and not work, or the regional anesthesia may not numb the intended area. Serious complications can also occur. These include bleeding, infection or nerve injury, but these are very rare. Your surgeon and anesthesiologist will check to make sure you are comfortable before, during and after the procedure. Do not hesitate to tell them if you are not.
Cortisone Shot
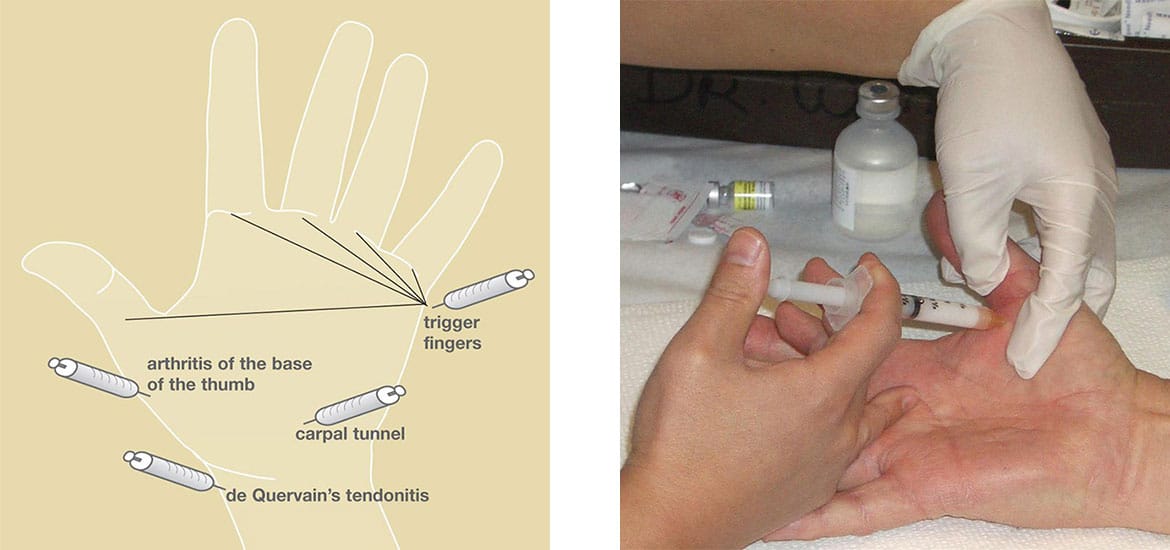
Figure: Cortisone injection sites & The cortisone shot is given with a small needle.
A cortisone shot can be used to treat some problems in the arm and hand. These can include trigger fingers, tendonitis, carpal tunnel syndrome, arthritis, tennis elbow and rotator cuff tendonitis. These injections usually contain a numbing medicine.
Cortisone is a steroid normally produced by your body, and it is a powerful anti-inflammatory. Corticosteroids tend to shrink, thin and slow things down. These steroids are different from anabolic steroids, which have been abused by athletes to build muscle and enhance performance.
Results
The cortisone shot should take effect within a few days, and the benefits can last for many weeks; however, results are not the same for everyone or every problem. For some conditions, one injection solves the problem. For others, several injections may be required. There is no set rule as to how many injections a person can get. Your doctor might limit the number of injections because repeated cortisone can damage tendons and/or cartilage.
Side Effects
The most common side effect of a cortisone shot is known as a “flare.” This pain is felt for one or two days after the injection. It can be treated with ice and by resting the area injected.
Other side effects might include:
- A rise in blood sugar level for diabetic patients for about five days
- Thinning of the skin
- “Lightening” of the skin at injection site (more common in patients with dark skin)
- Weakening of tendons, making them more likely to rupture
- Allergic reactions (rare)
One of the rare but more serious problems is an infection, especially if the injection was given into a joint. If you notice redness, extreme pain or heat at the injection site, or if you have a fever greater than 101° after an injection, you should call your doctor.
Hand And Finger Exercises
These common hand and finger exercises are typically recommended by a hand therapist or a hand surgeon. They may be helpful in recovering after surgery, to relieve pain or to regain mobility. These helpful videos can serve as a guide as you work through your exercises; however, please consult your hand therapist or hand surgeon before performing any of these exercises. Your provider(s) should also specify the number of sets and reps necessary, as well as how many times per day you should complete these exercises.
Differential Tendon Gliding
- Begin with your wrist supported and your fingers straight.
- Bend your bottom knuckles so your fingers are in a table top position. Return to straight.
- Bend your top two knuckles, trying to touch the top of the finger to the bottom. Return to straight.
- Make a loose fist, keeping your thumb out to the side. Return straight.
- Bend your bottom two knuckles, trying to reach for your palm.
Reverse Blocking
- Begin with the elbow supported.
- Keeping your involved hand relaxed, use your other hand to gently bend the bottom joints of your fingers (MP joints) to 90 degrees, if able.
- Maintaining this position, straighten the middle and end joints of all of your fingers. Hold for 10 seconds, then relax your fingers to your palm.
Make sure to keep your wrist straight during the exercise and maintain the bottom joints (MP) in flexion.
DIP Joint Blocking
- Begin by supporting your involved hand with the palm up. Use your other hand to support your involved finger just below the end joint.
- Bend and straighten the end joint, holding each position 3-5 seconds.
Support the middle joint only enough so that is does not bend. It is okay if the other fingers move during this exercise.
PIP Joint Blocking
- Begin by supporting your involved hand with the palm up. Use your other hand to support your involved finger just below the second joint, supporting over the last finger segment. The bottom (MP) joint should be straight.
- Bend and straighten your finger at the middle joint only. Hold position for 3-5 seconds and then return straight.
The end joint may also bend during the exercise. It is okay if the other fingers move as well.
Wrist Flexion and Extension
- Begin by supporting the involved forearm with your opposite hand.
- Keep your fingers relaxed in a light fist, and slowly bend your wrist back and forth.
Your fingers should be relaxed through the movement.
Wrist Radial and Ulnar Deviation
- Begin by supporting your forearm with the opposite wrist. Your fingers should be relaxed and your wrist in a straight position.
- Slowly bend your wrist from side to side, keeping your hand flat.
Try to keep your forearm stable while you move your wrist.
Wrist Circumduction – Alphabet Writing
- Begin by supporting your forearm with your opposite hand just below your wrist. You can rest your elbow on the table for added support.
- Keeping your fingers in a loose fist, practice writing the capital letters of the alphabet in the air, with the movement coming from your wrist.
- As the movement becomes easier, make the letters smaller and more precise.
Hand Therapy

Hand Therapy is a type of rehabilitation performed by an occupational or physical therapist with patients that suffer from conditions affecting the hands and upper extremities. Therapy enables patients to hasten their return to a productive lifestyle.
Patients who are candidates for hand therapy may have been affected by an accident or trauma leaving them with wounds, scars, burns, injured tendons or nerves, fractures, or even amputations of the fingers, hands or arms. Others include patients who suffer from conditions such as carpal tunnel syndrome and tennis elbow as well as from chronic problems such as arthritis or a neurologic condition (i.e. stroke).
What Does Hand Therapy Provide?
Hand therapy can provide the following:
- Treatments without an operation
- Help with recent or long-lasting pain
- Help to reduce sensitivity from nerve problems
- Learning to feel again after a nerve injury
- Learning home exercise programs to help with movement and strength
- How to make splints to help prevent or improve stiffness (Figure 1)
- Learning to complete everyday activities with special tools
- Help getting back to work
If surgery is needed, hand therapists can also help with a patient’s recovery. This may include assistance with helping wounds heal, preventing infection, scar treatment and reducing swelling.
Getting Back to Work
Hand therapists are able to talk with employers about preventing problems for workers with hand or arm symptoms. They may recommend changes at your place of work or different ways of doing your job to help ensure a healthy style of work.
Find a Hand Therapist
Search for a hand therapist in your area by going to www.asht.org, the official website of the American Society of Hand Therapists.
Heat Treatment And Cold Treatment

Applying a heat treatment or cold treatment is a common method for treating injuries, stiffness, swelling and pain. When used for fingers, hands and wrists, it can be very helpful for:
- Recent injuries (bruises or fractures) or chronic injuries
- Swelling
- Stiffness
- Irritation
Treatment
Benefits of a Heat Treatment
Heat or warmth will help get things moving by speeding up the molecules in tissues and increasing blood flow. Heat is helpful for stiff joints and muscles and can be useful prior to an activity. We often see an athlete warming up before a workout.
A warm shower or bath can help sore, stiff joints, especially in the early morning. A warm compress or heating pad can also relieve stiffness (Figure 1); however, too much heat could cause fainting, swelling, or burns to skin and tissues, so use your heat treatment in moderation
Benefits of a Cold Treatment
If there is pain, swelling, and irritation after an activity, cold treatment can reduce these symptoms. Cold slows down the molecules in tissues and reduces blood flow.
The most common cold treatment is ice or something that has been made cold by placing it in the freezer, such as a gel pack (Figure 2). Apply ice for 15 minutes, then allow a 15-minute rest before reapplying.
As with heat, too much cold can slow down and stiffen sore joints, so use this treatment in moderation. Applying ice or anything extremely cold to bare skin can cause injury. Always wrap the source of cold in some sort of fabric. If a bandage or splint is too thick and the cold is not getting through, apply the cold near the area on exposed skin. Stop using ice if you feel extreme pain or numbness due to the cold.
Special Treatments
Some special and more advanced heat or cold treatments may be used under the supervision of a therapist or physician. Some options may include:
- Therapeutic ultrasound: A qualified therapist will use ultrasound to slowly heat deeper tissues to help motion.
- Contrast bath: This is a bath that involves alternating heat and cold.
- Paraffin wax or warm wax: This can be used to apply heat via machines that are highly regulated and use a wax mixture that avoids skin burns.
Use caution when implementing a heat treatment or cold treatment. Monitor time and the condition of your skin, and always test the hot or cold item before applying. Contact your physician or therapist for assistance.
Pain Medication: What Are Opioids?
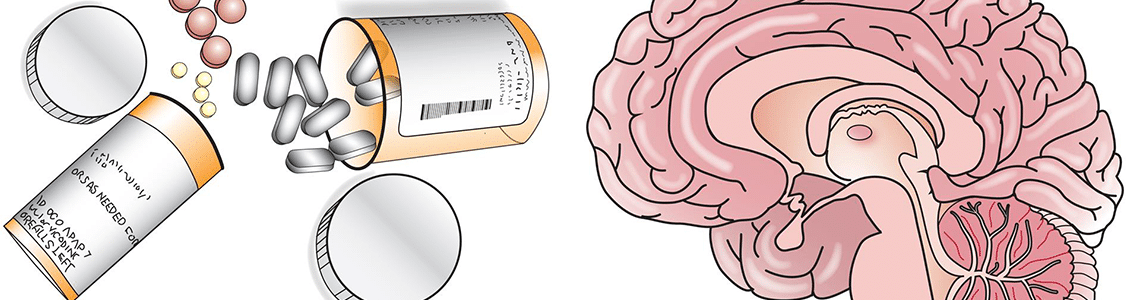
Opioids are a type of pain medication made from the poppy that is used to make opium and heroin. People have used them to treat pain for thousands of years. They are effective for treating acute pain involving skin, muscle, or bone and joint pain in the first several weeks following injury or surgery and are less effective for treating chronic pain, headaches or nerve pain. They are sometimes used to treat cancer pain at the end of life. Some of the most common such pain relievers used today include hydrocodone, oxycodone, hydromorphone, tramadol and codeine.
Misuse of Opioids: A large and growing problem
Over the last 15 years, the prescription of opioids has increased tenfold. Misuse now kills more than 100 people each day in the United States. It is responsible for more deaths than both suicide and motor vehicle collisions combined. According to the Food and Drug Administration (FDA), nearly 16,000 Americans died from overdoses involving these pain relievers in 2009. Most of these deaths were accidental.
The pain dilemma
Pain is expected after injury or surgery, and mindset matters. Pain relievers cannot take pain away; they just make the pain less bothersome. Patients quickly develop tolerance to these drugs, which means it requires more medicine to achieve the same amount of pain relief as time goes by. This is why such pain relievers work well in the short term, but do not work for long-term chronic pain.
Recreational use
Opioids are sometimes used by patients or their friends to get high. Over half of the teens abusing these medicines get them from family or friends without their knowledge. In addition to potential poisoning, recreational use creates addiction. One study of heroin users found that 39% of addicts reported being “hooked” on prescription pain relievers first.
Signs and Symptoms
The most common side effects of opioids are nausea, constipation, itching and drowsiness. The most serious effect is a decrease in breathing, which can result in death. The chance of death can increase when pain relievers are used together with alcohol or other drugs that make you sleepy.
Treatment
The progress of your treatment and your medication needs should be discussed with your providers, including your surgeon, physician assistant and nurse. While your providers want to limit pain following surgery or injury, they also understand the risks of abuse, addiction and possibly death associated with the use of these medicines. To reduce these risks, your provider may suggest switching to over the counter medicines such as ibuprofen or ancedimenifin once the initial intense pain subsides.
Disposal
Opioids should be disposed of when they are no longer needed to treat the injury or surgery for which they were originally prescribed. Studies report that between 10% and 30% of these pain relievers sold go unused. Leftover pain medicines kept in a patient’s home increase the risk of accidental poisoning and drug abuse. These tragedies often affect family members or friends.
Many communities have organized ways to dispose of unused pain relievers. Some law enforcement agencies have drop boxes or hold designated dates to collect unused prescription medicines. Do not flush the pills down the toilet because it releases the drugs into the waterways. Water treatment facilities do not effectively remove these dissolved drugs, so contamination of drinking water is a growing concern.
Pain Management After Surgery
Pain Management: How To Get Pain Relief
Pain after an injury or surgery is common. There are many ways to manage and reduce this pain that may or may not include medication. Each patient, surgery, and surgeon are unique, and the approach to pain management is different for everyone.
Discuss your concerns and expectations about pain with your surgical team before surgery. They do not want to see you in pain! Asking questions and creating a plan can improve your experience. Your surgical team will have specific recommendations for you. Use this page as a general guide to discuss with your care team what methods will work for you.
Surgery Day
Before surgery, a nerve block can be given to numb the surgical area. A nerve block is an injection that can block pain to a certain area. Either your surgeon or anesthesia provider may perform this. A block may reduce the amount of medication you need during and after surgery. As your surgery begins, you may receive medications by mouth or IV to dull the pain. Your care team will give you an appropriate amount of medicine during surgery to keep your pain under control, even if you are asleep. Learn more about the different types of anesthesia you may receive. You may also receive medication in the recovery room after surgery.
Post-Surgery Pain Management
While always important to follow your doctor’s instructions, here are some different methods that your team may recommend to reduce your pain:
- Elevate: Inflammation and fluid will run to the site of surgery like water flowing down a hill. Elevating the injured area so it is higher than your heart can reduce swelling and pain by bringing the fluid away. Swelling can increase quickly by putting your hand at your side, and this can make your dressing feel tight.
- Loosen your dressing: If your dressing/splint feels tight, and elevation for 10 minutes does not improve the tight sensation, contact your surgical team. It may be recommended that you unwrap any tape or elastic wrap and loosen the outer bandage. If this does not help, you may be advised to tear, unwrap, or cut the inner layers with blunt-tipped scissors. Make sure you are cutting on the opposite side of where your incision is located. When done, you will need to try to rebuild your dressing to keep your wound clean and covered. Before doing any of this, check with your medical team.
- Keep moving: If allowed by your surgeon, try to frequently move the fingers, wrist, elbow, and/or shoulder that are outside of the splint or cast. You can do this gently and slowly. This improves blood flow. It may be uncomfortable to move at first, but the discomfort will improve with time and motion. Your surgeon will be more specific about what to move and what to rest.
- Ice the area: Icing the painful area will reduce swelling, inflammation, and pain. There may be certain procedures (such as surgery on arteries, skin grafts or flaps) where a cold treatment could be harmful, so consult your surgeon before using ice.
- Heat the area: If you are in the phase of care where you can remove your dressing or splint, you may be able to try heat. Heat increases blood flow to an area and can help with muscle spasms, muscle soreness and joint pain.
- Avoid smoking: Chemicals present in cigarettes can increase pain. Reducing or quitting smoking can improve your pain. Nicotine alone can cause pain by reducing blood flow. For elective surgery, it is best to stop or limit smoking at least 2 weeks before your date.
Post-Surgery Medication Management
The methods listed above are often effective when used in combination with taking medications post-surgery. There are many different classes of medication that can help pain. Some can be purchased over the counter, and some require a prescription. Your surgical team will help create a plan with you. Some commonly prescribed medications can include:
- Tylenol (Acetaminophen)
- Aleve (Naproxen)
- Motrin/Advil (Ibuprofen)
- Celebrex (Celecoxib)
- Toradol (Ketorolac)
When taking medication, keep the following in mind:
- It may take 30-60 minutes for your body to absorb the medication after you take it by mouth, so be patient.
- Longer-acting medications used before bedtime may help you sleep better the first few nights after surgery.
- The first few nights post-surgery will generally be the toughest.
- Do not exceed the dose recommended by your physician or combine medications without consulting with your physician.
If you are unfamiliar with these medications, your surgeon can specify how much medication you should take, for how long, and how often. It is important to follow the directions of your surgeon carefully.
Opioids
Opioids are a type of pain medication made from the poppy plant that is used to make opium and heroin. They can be effective in treating pain, but opioids should be used as a last resort, in limited amounts, and for as short of a time as possible. Use of these medications should only be done under the guidance of your doctor. When taking opioids, you are at risk of becoming dependent on the medicine, and they may become less effective over time.
Oxycodone and hydrocodone are two of the most commonly used a opioid “pain” pills. Your pill may already have acetaminophen combined with the pain medicine, so make sure you are not taking too much if you take this separately. Your surgeon will give you a customized plan for managing your pain based on your type of surgery, number of procedures, duration of surgery, etc. Overdoses of pain medications can be dangerous and life-threatening.
Scar Treatment

Figure (Left) : Silicone gel can be placed on a scar for treatment. Figure (Right): The different phases of a scar are shown here.
Scar formation is a normal response following any injury or surgery; it is the way the body heals injured structures. Scar tissue may involve only the superficial skin, or it may involve the deeper tissues beneath the skin, including nerves and tendons.
An active scar may be red, raised, firm and thick. Scars can become overly sensitive and can limit motion and function.
Treatment
Your hand surgeon or hand therapist may recommend a variety of scar treatments once your injury is healed, cuts are closed, and stitches are removed. Timing of your scar treatment varies depending on the type of injury or surgery. Scar management treatments may include:
- Scar massage can help decrease sensitivity and loosen any deeper areas that seem “stuck.” Scar massage helps to produce a smooth, moveable scar. You can use any type of over-the-counter cream such as Vaseline, cocoa butter or hand lotion for this. The tissue should be massaged in the direction of the scar for ten minutes twice a day. This is useful for 3-6 months or for as long as it seems to be helping.
- Early controlled exercise programs can prevent stiffness of nearby joints and keep tendons gliding under the skin.
- Silicone gel can be placed on the scar in sheets or in liquid form (Figure 1). Silicone sheets can be washed and re-used. Silicone gel dries as a very thin layer and will stay on curved skin surfaces that move throughout the day. Silicone therapy is best used 12-24 hours a day for 3-6 months. Taping/wrapping of the scar can help reduce swelling and tension.
- Massage, vibration and rubbing the scars with various textures can help overly sensitive scars. These occur when the nerves in the skin and deeper tissues are affected by the injury or surgery. The scar may also be submerged in slightly abrasive particles. The goal of this is to reduce scar sensitivity and to help the skin and nerves become tolerant of the normal forces of everyday living. This process of “desensitizing” the scar can take up to 4 months. It can be started as soon as the skin and repaired tissues have healed.
- Injections or surgery can be effective for special scar problems. Burn scars or other more serious injuries can require aggressive treatment. Special gloves or topical treatment may be used for burn scars.
Some scars take up to a year to mature. Therefore, some scar revisions (a surgery that minimizes a scar so it blends in) may not be offered until a year after injury/surgery. Scars have completed the healing process when they are light in color, smooth, and no longer sensitive to touch. A fresh, healing scar (pink, red, raised, thick, and sensitive) should be protected from sunlight; sun exposure can darken it.
Scar Healing
After the skin and deeper tissues have healed, the scar goes through four different stages of healing. Although the initial skin scar may be minimal, the scar will often enlarge and become more reddened over the following 4-6 weeks. An active scar is typically red, raised, firm and thick. Sometimes this change can be confused with infection. Also, the outermost layer often loosens while the deeper layers remain intact; this is normal as well.
Following the swelling/reddening phase, the wound becomes smaller and paler over the next 2-3 months (Figure 2). Later, the scar becomes soft and has a more natural color in most individuals.
Splint and Cast Care
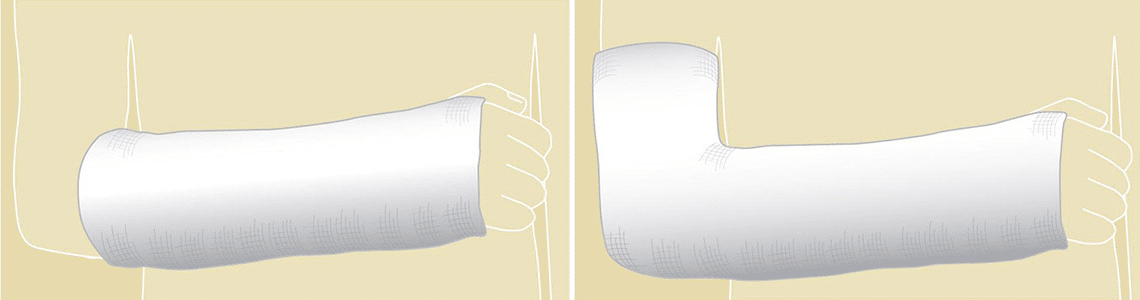
Figure (Left): Short arm cast, below elbow & Figure (Right): Long arm cast, above elbow
Splints and casts are supports that are used to protect injured bones and soft tissues. An arm cast completely encircles the limb with a hard, rigid outer shell (Figures 1 and 2). A splint provides rigid support along just a portion of the limb, with soft or open areas in between (Figures 3 and 4). Splints are often used in the immediate post-surgery or injury phase. This is because a splint can better allow for the swelling that often occurs in these situations. Your doctor will decide which type of support is most appropriate for you and your arm condition.
Arm Cast Materials
An arm cast is made with plaster or “fiberglass” to form the hard, supportive outer layer. Fiberglass is lighter, more durable, and “breathes” better than plaster. Some fiberglass casts are also waterproof, depending on the underlying padding material (ask your doctor if such a cast is appropriate and available for your treatment). Plaster is less expensive and shapes better than fiberglass. Both materials have their place in treating arm injuries and protecting the arm after surgery. Also, both materials are dipped in water to start the setting process. Most casts also have a soft lining of cotton or similar material for padding underneath the hard material. X-rays can be taken through casts, but casts do block some of the x-ray detail.
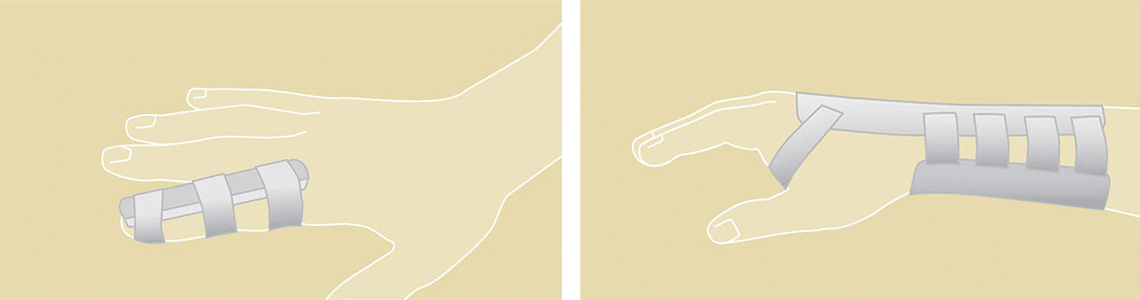
Figure (Left): Finger splint & Figure (Right): Wrist splint
A splint can be made with these same materials or with plastic, fabric, or padded aluminum. They can be custom-made, or they may be pre-made. They come in a variety of shapes and sizes, depending on the specific need. They often have Velcro straps or similar closure systems, and this makes them easier to take on and off.
Treatment
How to take care of your arm cast or splint
Keep your cast or splint clean and dry unless it is made to be waterproof. Being in contact with damp padding can irritate your skin. Plaster gets softer and weaker when it gets wet. Here’s how to keep it dry:
- Use plastic bags or a waterproof cast cover to keep your splint or cast dry when bathing. Seal the bag with tape or rubber bands so there is a water-tight seal.
- Elevate your hand in the shower above your head to avoid water running under the seal and into your cast.
- Remove the bag or cover afterward. Do not keep it constantly covered because moisture may build up from normal sweating.
Follow these additional rules when wearing an arm cast or splint:
- Do not let dirt, sand, or other materials get inside of your splint or cast.
- If you feel itching, do not place anything inside your cast because you can injure your skin; ask your doctor for advice.
- Never trim the cast or splint by yourself. If there are rough edges or if your skin gets irritated around the edges of the cast, notify your doctor, who has the proper tools to fix it.
If your cast or splint develops cracks or soft spots, contact your doctor to see if it needs to be repaired or changed.
How to take care of a waterproof cast
Waterproof casts can be submerged in water, although it is best to avoid water from lakes, rivers and oceans because your skin can become irritated if dirt or sand gets inside the cast.
Follow these additional rules to take care of your waterproof cast:
- When you come in contact with chlorinated water or dirty water, rinse the cast with fresh water when done.
- Allow the inside of the cast to drain as much as possible after it gets wet. If you have a cast that goes past your elbow, be sure to drain the area around the elbow well. The rest of the water will evaporate.
- Consider rinsing the cast with clean water after excessive sweating (although sweat will not harm the cast liner).
CAST REMOVAL
Never try to remove a cast yourself; you may cut your skin or prevent proper healing of your injury. A cast should be removed only by a professional with the proper tools and training. Casts are removed with a special type of saw that will not cut your skin.
Remember, a cast is there to protect you while your injury heals. It is only a temporary inconvenience, with the goal of helping you recover.






